A safety culture is the collective effort of an institution to direct its resources towards the goal of safety.
Material and methodsAn analysis is performed on the six years of experience of the Committee on the Safety of the Neonatal Patient. A mailbox was created for the declaration of adverse events, and measures for their correction were devised, such as case studies, continuous education, prevention of nocosomial infections, as well as information on the work done and its assessment.
ResultsA total of 1287 reports of adverse events were received during the six years, of which 600 (50.8%) occurred in the neonatal ICU, with 15 (1.2%) contributing to death, and 1282 (99.6%) considered preventable. Simple corrective measures (notification, security alerts, etc.) were applied in 559 (43.4%), intermediate measures (protocols, monthly newsletter, etc.) in 692 (53.8%), and more complex measures (causal analysis, scripts, continuous education seminars, prospective studies, etc.) in 66 (5.1%). As regards nosocomial infections, the prevention strategies implemented (hand washing, insertion and maintenance of catheters) directly affected their improvement. Two surveys were conducted to determine the level of satisfaction with the Committee on the Safety of the Neonatal Patient. A rating 7.5/10 was obtained in the local survey, while using the Spanish version of the Hospital Survey on Patient Safety Culture the rate was 7.26/10.
ConclusionsA path to a culture of safety has been successfully started and carried out. Reporting the adverse events is the key to obtaining information on their nature, aetiology and evolution, and to undertake possible prevention strategies.
La cultura de seguridad es el esfuerzo colectivo de una institución para encaminar la totalidad de los recursos hacia el objetivo de la seguridad.
Material y métodosSe analizan 6 años de experiencia de la Comisión de la Seguridad del paciente neonatal. Se creó un buzón para la declaración de acontecimientos adversos y se diseñaron medidas para su corrección, así como información del trabajo realizado y su valoración.
ResultadosDurante 6 años se han recibido 1.287 notificaciones de acontecimientos adversos de las cuales 600 (50,8%) ocurrieron en la UCI neonatal. Quince (1,2%) graves contribuyeron a la muerte del paciente; 1.282 (99,6%) acontecimientos adversos se consideraron evitables. Se adoptaron medidas correctoras simples (notificación, alertas, etc.) en 559 (43,4%), medidas intermedias (protocolos, boletín, etc.) en 692 (53,8%) y medidas más complejas (análisis causa-raíz, libretos, formación continuada, trabajos prospectivos, etc.) en 66 (5,1%). Respecto al trabajo sobre las infecciones relacionadas con la asistencia sanitaria, se demostró cómo las estrategias de prevención (lavado de manos, inserción y mantenimiento de vías) repercuten directamente en su disminución. Se realizaron 2 encuestas, obteniendo un grado de satisfacción de la comisión de 7,5/10. Con la versión española del Hospital Survey on Patient Safety Culture se obtuvo un grado de cultura de seguridad de 7,26 sobre 10.
ConclusionesSe ha iniciado un camino hacia la cultura de seguridad. La declaración de los acontecimientos adversos es un elemento clave para obtener información sobre el tipo, la etiología y la evolución, y decidir posibles estrategias de prevención.
Quality of care, according to Avedis Donabedian, is the expected model of health care to maximise the level of patient welfare, once the balance of benefits and losses expected in every phase of the care process has been assessed.1 According to the Council of Europe, it is the degree to which the treatment dispensed increases the patient's chances of achieving the desired results and diminishes the chances of undesirable results, according to current knowledge.2 There are various different definitions of this term, describing the concept according to a series of criteria, such as effectiveness, efficiency, appropriateness, equity, safety, respect, prevention, continuity, coordination, etc.3–7
Patient safety (PS) means reducing the risk of unnecessary harm associated with health care to an acceptable minimum according to current knowledge, available resources and the context in which the care is provided. Concern for PS can be regarded as an international movement involving all the agents that provide health services, from health policy planners to health care professionals.8 Safety is an important component of the definitions of quality proposed by Donabedian, the Institute of Medicine and the Joint Commission (JCAHO).1,4,6
In the JCAHO's view, the essential basis of PS is health care error prevention, which must be managed proactively, identifying the risk and the changes that need to be applied to reduce it, determining who is responsible for implementing each of the planned actions, when each action should be carried out and what method should be used to assess their efficacy.9 A necessary prerequisite is that health care culture should evolve towards a culture of safety that looks for the weaknesses in the system instead of blaming the individuals who work in it.
The culture of safety is the set of values, attitudes and behaviours in an organisation that are directed to making its activities safe for its clients, by creating methods of work that promote them. This culture is essential in health care quality management; for this reason it has been incorporated into health care organisations and is a priority when it comes to developing a proactive health care risk management system that detects problems before they occur. A culture of safety requires an information system to collect, analyse and distribute the information related to incidents, and this in turn requires 4 subcultures: a culture of communication, whereby staff perceive a climate of confidence for communicating incidents; a culture of fairness, in which unacceptable conduct that will not be tolerated is clearly distinguished from that which, though wrong, is understood and accepted; a culture of learning, characterised by a desire to analyse and draw conclusions; and a culture of flexibility, willing to implement change. A team has a good culture of safety when the professionals belonging to it are aware that it is possible to make mistakes and are constantly on the alert, capable of identifying and recognising errors, learning from them and taking the appropriate measures to correct them, with the aim of making patient care safer.10
This concept led to the creation of the Neonatal Patient Safety Committee (NPSC) in the Neonatology Service of the Hospital Clínic in Barcelona. In this article we present its first 6 years’ experience.
Material and methodsThe NPSC was created in January 2008. It is made up of 3 medical professionals and 6 nursing professionals from the Neonatology Service, serving on a voluntary basis, who meet once per month.
The NPSC's work began with a clinical session consisting of a wide-ranging review of the literature on the subject. The concepts of health care risk and adverse event (AE) were introduced to replace the terms blame and medical error. The committee set out the magnitude of the problem and the importance of reinforcing the values which constitute the basis of the culture of safety, such as shared responsibility, teamwork, training, patient-centred care and prevention.
One of the strategies for reducing health care risk was to have a drop box for voluntary and anonymous reporting of AEs, so as to become aware of them, analyse them and put measures in place to prevent them from recurring. In our Unit protocols are reviewed, discussed and agreed every week. As a result of the AEs reported, new protocols were produced or existing ones revised. A quarterly session on PS is included in the service's continued training programme and the members of the NPSC normally attend the one-day conferences on PS organised by the Catalan Regional Government (Generalitat de Catalunya) (so far 9 conferences have been held).
To ensure that information is transmitted properly, an email contact group of all staff was created, and also a monthly newsletter, “For Safer Health Care”, consisting of an editorial and articles on safety, new protocols, improvements, alerts, etc., and a web page within the Hospital's Intranet, containing information on the NSPC.
Results- 1.
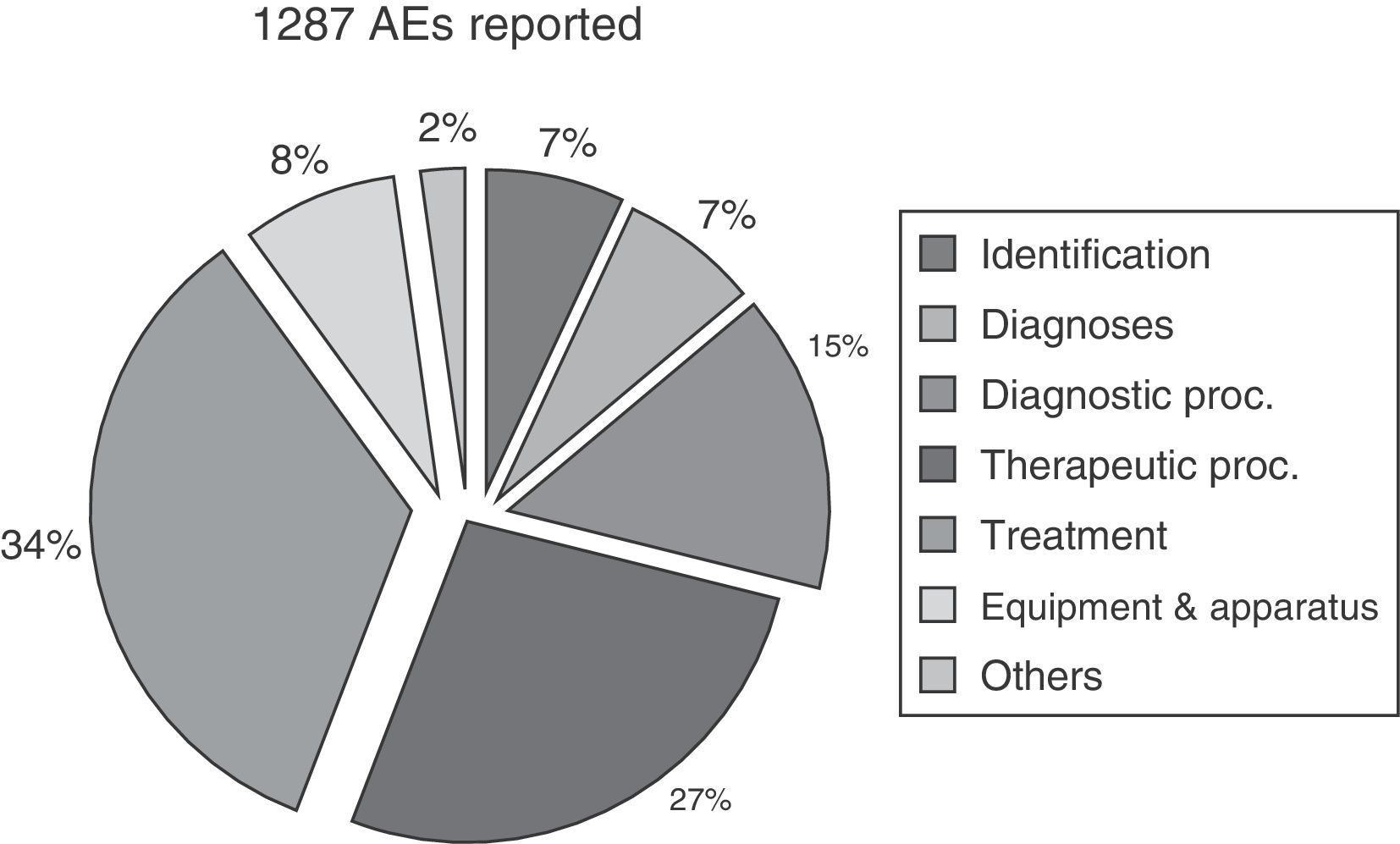
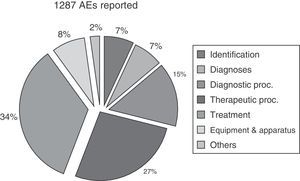
Analysis of the AEs reported. From 1 February 2008 to 31 March 2014, 1419 notifications were received in the drop box, 132 of which were not related to a specific AE but reflected various problems, such as patient overload, lack of material, etc. There were therefore 1287 remaining AE notifications, distributed, according to the various health care issues involved, as shown in Fig. 1. Of these, 1181 (91.8%) occurred in the neonatal unit, 600 (50.8%) of them in the intensive care unit (ICU). Only in 995 of the reports was the professional status of the informant stated, with 413 (32.1%) being reported by medical staff and 582 (45.2%) by nursing staff. In 15.3% of cases the informant was the person involved in the AE; 56.25% were by direct observation and in 28.43% this point was not specified. Only 307 reports stated the birth weight of the patient affected and in 72.6% of cases it was 1500g or less. A total of 99.6% of the AEs were considered avoidable.
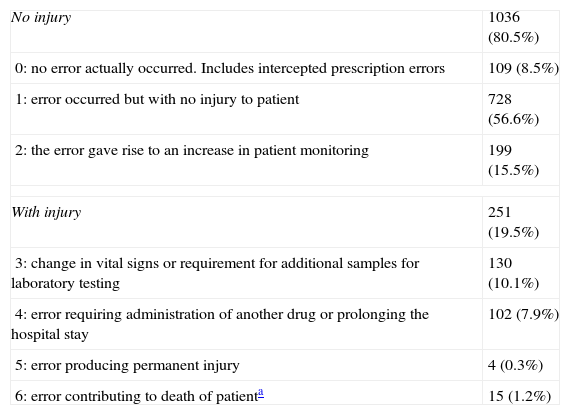
The AEs are presented in terms of their severity, according to the classification proposed by Hartwig et al.11 in Table 1. In the group of notifications with fatal consequences (1.2%) the patient's weight was between 500 and 1000g. In 2/3 of them the death was related to ventilation problems and catheters, and in 1/3 it was related to health care-associated infections (HAIs).
Table 1.Classification of adverse events by severity.
No injury 1036 (80.5%) 0: no error actually occurred. Includes intercepted prescription errors 109 (8.5%) 1: error occurred but with no injury to patient 728 (56.6%) 2: the error gave rise to an increase in patient monitoring 199 (15.5%) With injury 251 (19.5%) 3: change in vital signs or requirement for additional samples for laboratory testing 130 (10.1%) 4: error requiring administration of another drug or prolonging the hospital stay 102 (7.9%) 5: error producing permanent injury 4 (0.3%) 6: error contributing to death of patienta 15 (1.2%) Taken from Hartwig et al.11
aFive air leaks in extremely premature infants, one accidental extubation, 2 catheter accidents (one acute haemorrhage from the umbilical venous catheter leading to a state of shock and one severe intraventricular haemorrhage and a Silastic catheter with an intravascular rupture), 5 health care-associated infections, one diagnostic error and one of equipment or apparatus (extreme hypothermia in an extremely premature infant).
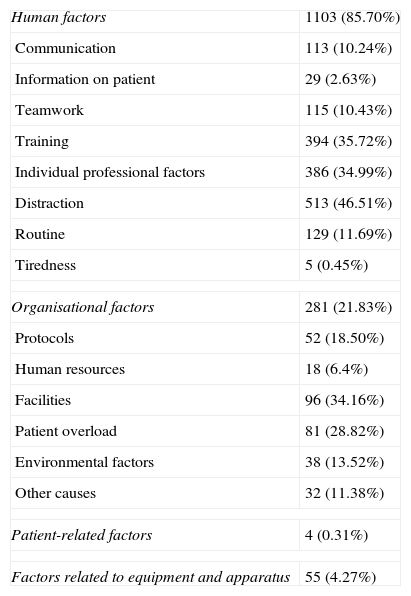
The possible factors connected with the AEs are shown in Table 2. Among the human factors, the most prominent were distraction, individual professional factors and lack of training, and among the organisational factors they were patient overload and problems with facilities.
Table 2.Possible causal factors for the AEs reported.
Human factors 1103 (85.70%) Communication 113 (10.24%) Information on patient 29 (2.63%) Teamwork 115 (10.43%) Training 394 (35.72%) Individual professional factors 386 (34.99%) Distraction 513 (46.51%) Routine 129 (11.69%) Tiredness 5 (0.45%) Organisational factors 281 (21.83%) Protocols 52 (18.50%) Human resources 18 (6.4%) Facilities 96 (34.16%) Patient overload 81 (28.82%) Environmental factors 38 (13.52%) Other causes 32 (11.38%) Patient-related factors 4 (0.31%) Factors related to equipment and apparatus 55 (4.27%) Taking into account the total number of newborns (NBs) hospitalised during the study period (4065 in all and 1951 admitted to the ICU), the proportion of AEs reported was 0.29 AE per NB hospitalised and 0.31 AE per NB admitted to the ICU.
- 2.
Root cause analysis of severe cases (tracheal perforation in an extremely premature infant, umbilical catheter securement method, endotracheal tube suctioning, intravenous infusion of milk, traumatic bladder catheterisation, etc.).
- 3.
Measures adopted after analysis of the reported AEs. Simple corrective measures were adopted in response to 559 (43.4%) of the AEs: direct notification, safety alerts, correct labelling of infusion pumps, computerised medication labels, posters, checking of material, calibration of electrical medical equipment, etc. The main intermediate corrective measures in relation to 692 (53.8%) of the AEs were formulation of clinical protocols and procedures, clinical sessions, a monthly newsletter, a poster competition on prevention of HAIs, etc.
In 5.1% of the AEs more complex measures were required:
- –
Booklets that were easy to use, laminated and very visual, explaining some of the service's procedures: securing the airway, assisted ventilation, administration of intravenous drugs, etc.
- –
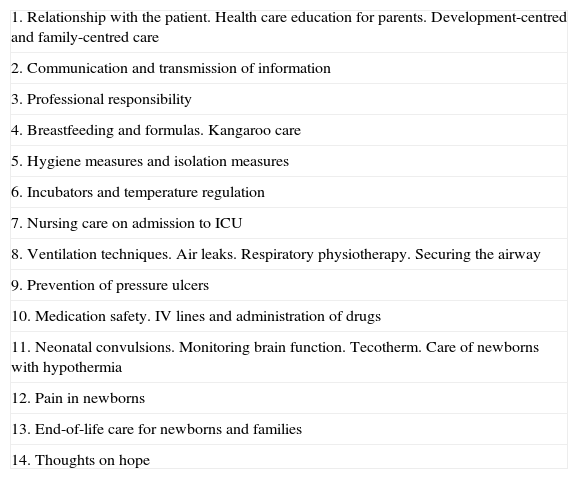
Annual continued training sessions to correct detected weaknesses. Five sessions were held, 24 tutors, 67 trainers and 250 attendees participated, and a range of subjects related to day-to-day neonatal practice were addressed (Table 3). In the overall course assessment a mark of 3.73 out of 4 was obtained.
Table 3.Subjects covered in the continuing training course.
1. Relationship with the patient. Health care education for parents. Development-centred and family-centred care 2. Communication and transmission of information 3. Professional responsibility 4. Breastfeeding and formulas. Kangaroo care 5. Hygiene measures and isolation measures 6. Incubators and temperature regulation 7. Nursing care on admission to ICU 8. Ventilation techniques. Air leaks. Respiratory physiotherapy. Securing the airway 9. Prevention of pressure ulcers 10. Medication safety. IV lines and administration of drugs 11. Neonatal convulsions. Monitoring brain function. Tecotherm. Care of newborns with hypothermia 12. Pain in newborns 13. End-of-life care for newborns and families 14. Thoughts on hope - –
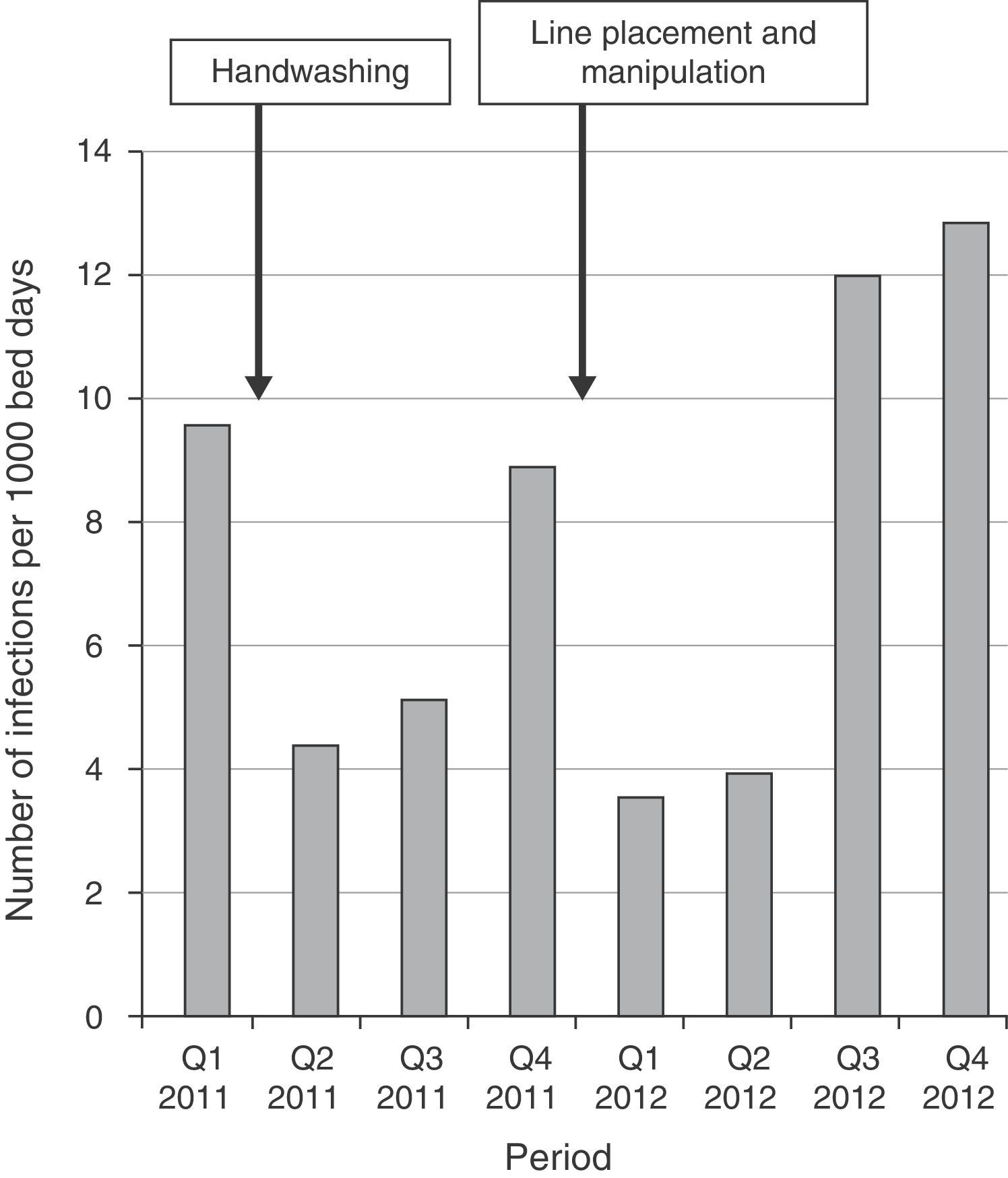
Prospective work on HAIs. Two lines of strategy were pursued: proper handwashing technique and line placement and maintenance technique. Five teams were responsible for producing or updating protocols and carrying out subsequent staff training. A total of 23 professionals (nurses and neonatologists) took part. The evolution of the HAI rate during the two years the work lasted was assessed. Before the work began the incidence of HAIs was 10.7 per 1000 days of hospitalisation.
- •
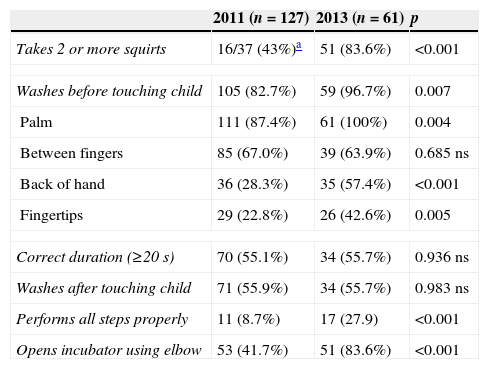
On proper handwashing technique, the training was carried out during the first 2 months of the year, improving compliance with the procedure from 8.7 to 27.92% (p<0.001) (Table 4). HAIs decreased from 9.64 per 1000 bed days to 4.41 between the 1st and 2nd quarters, subsequently increasing to 5.16 and 8.91 in the 3rd and 4th quarters (Fig. 2).
Table 4.Assessment of handwashing technique in 2 periods.
2011 (n=127) 2013 (n=61) p Takes 2 or more squirts 16/37 (43%)a 51 (83.6%) <0.001 Washes before touching child 105 (82.7%) 59 (96.7%) 0.007 Palm 111 (87.4%) 61 (100%) 0.004 Between fingers 85 (67.0%) 39 (63.9%) 0.685ns Back of hand 36 (28.3%) 35 (57.4%) <0.001 Fingertips 29 (22.8%) 26 (42.6%) 0.005 Correct duration (≥20s) 70 (55.1%) 34 (55.7%) 0.936ns Washes after touching child 71 (55.9%) 34 (55.7%) 0.983ns Performs all steps properly 11 (8.7%) 17 (27.9) <0.001 Opens incubator using elbow 53 (41.7%) 51 (83.6%) <0.001 - •
As regards line placement and maintenance technique, the protocols were reviewed, updated and distributed: antiseptics and disinfectants, correct use of gloves, placement and manipulation of lines (peripheral, umbilical and peripherally inserted central lines), parenteral nutrition and laminar flow hood. Immediately following the intervention the incidence of HAIs fell from 8.91 to 3.53 per 1000 bed days, subsequently rising again to 12.83 per 1000 bed days (Fig. 2).
- –
- 4.
Participation in round table discussions: papers, communications and posters were presented at conferences or meetings. A prize was won for best oral communication (“Strategy for improving PS in a Neonatology Service”) and 2 prizes for best poster (“Two years of notification of adverse events in Neonatology” and “Sentinel events: analysis and ethical reflection on health care safety”). Three studies were published.12–14
- 5.
Periodic evaluation of the work of the NPSC. In 2012 a quality survey on the NPSC was carried out. Replies were received from 23 professionals (48% of those surveyed) on: the usefulness of the NPSC (83% of the responses considered it useful or very useful), its transmission of information (91% considered it good or very good), the frequency of notifications of AEs (83% had reported them occasionally, quite often or very often; 17% had never reported any), the usefulness of the revised protocols (100% very useful), the usefulness of the continued training sessions on safety (96% considered them useful or very useful), the level of satisfaction with the NPSC (average rating: 7.5/10) and the level of satisfaction with the newsletter (average: 9/10; 100% read it).
- 6.
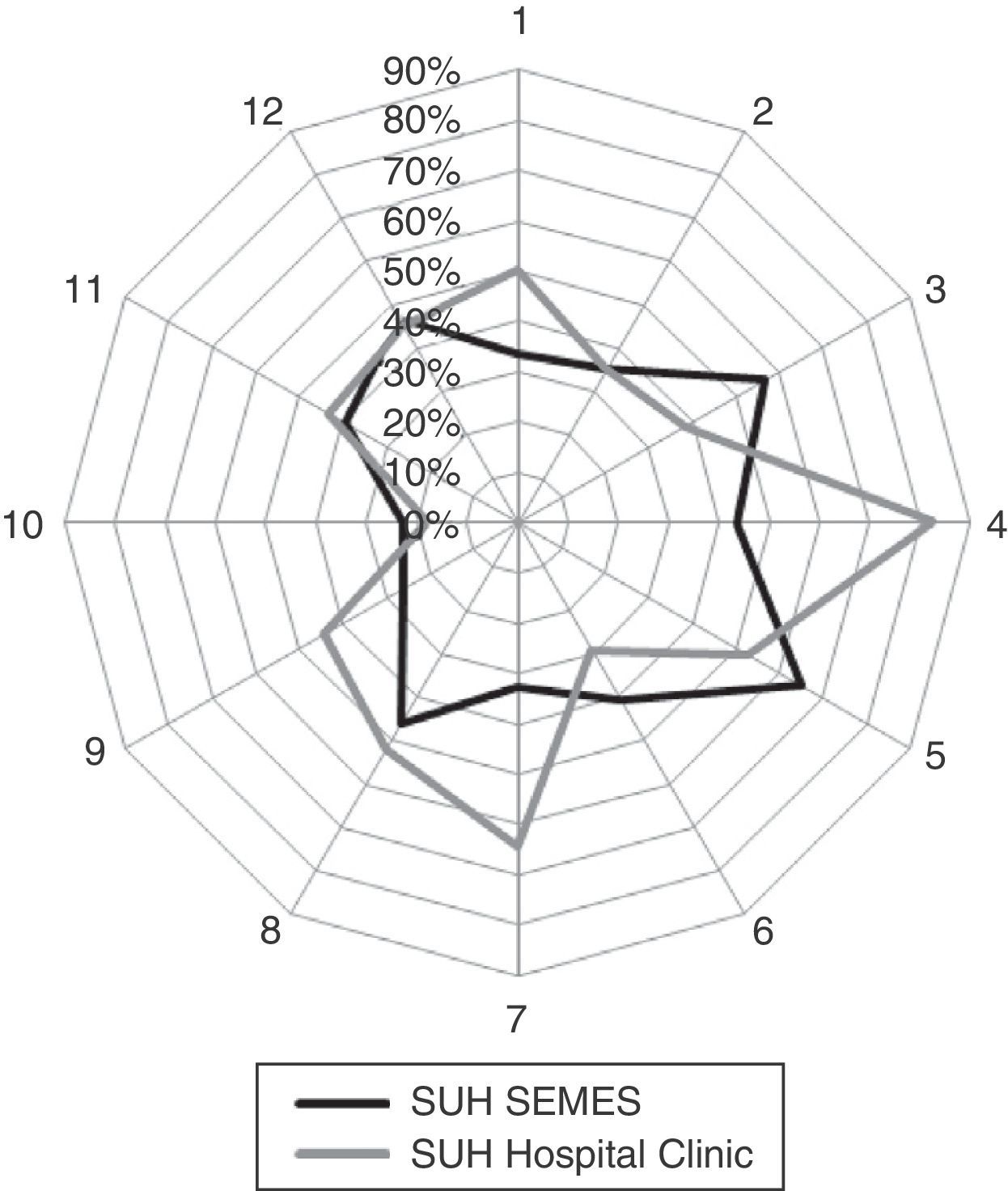
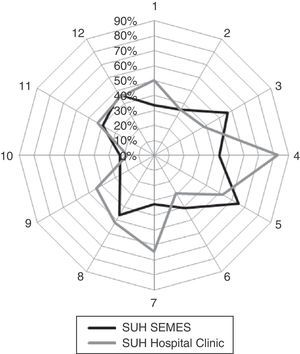
Comparison with other studies. In 2013 a Questionnaire on Patient Survey (a Spanish version of the Hospital Survey on Patient Safety15) was distributed, obtaining a level of safety culture of 7.26 out of 10, based on 30 responses (62.5% of those surveyed). Our service, compared with nearly 4000 surveys conducted on 71 hospitals in 14 autonomous communities all over Spain (a study carried out by the Spanish Society of Urgent and Emergency Medicine), was in 17th place. Benchmarking between our hospital and Spanish hospitals as a whole is shown in Fig. 3. We scored particularly well in organisational learning and continuous improvement, feedback and communication on errors, and frequency of reporting of events.
Figure 3.Study of positive responses compared with 71 Spanish hospitals analysed by the Spanish Society of Urgent and Emergency Medicine (SEMES). 1: frequency of reporting of events; 2: perception of safety; 3: expectations/actions of service or unit managers; 4: organisational learning/continuous improvement; 5: teamwork in the unit; 6: ease/openness of communication; 7: feedback and communication on errors; 8: non-punitive response to errors; 9: provision of human resources; 10: management support for patient safety; 11: teamwork between units; 12: problems at shift changes and interfaces of care.
A culture of safety is defined as the collective effort of an institution to direct all its resources (human, technological and organisational) towards the objective of safety.16 Health care safety is the result of designing structures and processes that reduce the likelihood of AEs occurring. According to the United Kingdom's National Patient Safety Agency, to build a safety culture you need to know the team's level of engagement with safety, highlight successes, be open and honest when things go wrong, apply the same level of strictness to all aspects of safety (reporting and investigating incidents, root cause analysis of significant AEs, complaints), protect professionals and ensure quality. Consolidating a culture of safety requires leadership, teamwork, responsibility, understanding, awareness that patient overload can increase risk, and an organisation that celebrates good practice, promotes training, encourages dialogue, reduces the impact of hierarchical relationships and ensures that its systems and procedures are safe.17
It is difficult to make a comparison with the various other existing studies in the literature, especially bearing in mind that AEs are under-reported and that the parameters selected to ascertain them are not the same: voluntary reporting,18–20 direct observation,21 studying claims22 and reviewing clinical histories,23–25 among others.26 In the last case the “trigger” methodology makes it possible to establish “alerts” which set an investigation in motion to determine whether or not an AE has taken place.27,28 All the methods have their advantages and disadvantages, but AEs are always underestimated. Sharek et al. analysed 749 clinical histories from 15 neonatal ICUs and found 841 AEs, of which only 8% had been reported.27 Taylor et al. conducted a survey on inclination to report: 34.8% stated that they had reported fewer than 20% of their own AEs in the last 12 months and 32.6% that they had reported fewer than 40% of the AEs observed among their colleagues.20 In our study it is notable that in only 15% (197) of the reports was the informant the person involved in the AE.
The incidence of AEs varies greatly according to the method used to detect them. In neonates it ranges between 0.13 and 0.74 per patient admitted, or 20 to 32 per 1000 patient days.18,19,24,25,27,28 In our study it was 0.29 per patient admitted. In the study by Sharek et al. it is equivalent to 0.74 AEs per patient, with a range of 0 to 11 AEs per patient.27 In a review of 3595 records Brennan et al. found 0.6±0.1 AEs per NB or 1.4%±0.3, according to the method used, on the basis of diagnosis-related group (DRG) risk.23 According to Kanter et al. it is 1.2 per 100 discharges in premature neonates29 and in a study by Ligi et al. it varies from 7.6 to 4.8 per 1000 patient days in NBs with a mean gestational age of 34–35 weeks, after the introduction of preventive strategies subsequent to analysis of incident reporting.30
Care of NBs is associated with a high risk of AEs because the physiological immaturity of their systems, the severity of their condition and the complexity of the treatments make them highly vulnerable. The rate of AEs is higher in patients with a gestational age of under 28 weeks and a weight less than 1500g23, and in children admitted to an ICU, and even higher the longer they are hospitalised.31 According to Sharek, the AEs most commonly identified were nosocomial infections (27.8%), catheter infiltrations (15.5%), abnormal cranial imaging (10.5%) and accidental extubations (8.3%).27 In the study by Kanter et al., 60% of them were procedural errors and 25% were medication errors.29 In the Brennan study, 2.6% caused permanent sequelae and 13.6% led to death.23 Our study shows a notably similar incidence, whether we take the unit as a whole or the ICU; however, all the AEs with fatal consequences affected extremely premature infants (500–1000g) admitted to the ICU. The cause of death was mostly related to ventilation problems (40%), catheters (13.3%) and HAIs (33%).
HAIs are so common that one could make the mistake of regarding them as inherent consequences of the low immunocompetence of NBs and the need for complex and prolonged invasive procedures, but nosocomial infections must be treated as severe AEs. The reduction in infections after training campaigns and maximising aseptic measures with strict handwashing, correct catheter placement technique and programmes such as Bacteremia Zero32 is irrefutable proof of this. Many factors influence the pathogenesis of complications in extremely premature infants, but their outcome will depend on correct management; one must be very strict about raising the awareness of staff serving in the neonatal ICU and training them, as a severe incident can unleash a cascade of undesirable events that lead inexorably to the child's death.
As for prevention of AEs, Barrionuevo and Essandi, in a review of 484 neonatal clinical records, detected 146 AEs, of which only 2.7% were considered nonpreventable25; in other studies the figure varies from 27.6 to 56%.23,30,33 In our study there is a strikingly high incidence of avoidable AEs, with 86% of contributory factors being related to the professionals and 22% related to the organisation; that is why efforts have been made in staff training and in producing and distributing guidelines, protocols, checklists, recommendations, automatic reminders, alerts, etc. The fact that only 0.31% of the factors detected were patient-related is because, since it is a neonatal unit with a high percentage of extremely premature infants, this element was not included as a specific risk factor.
No study can be carried out without being evaluated and a comparison made with other hospitals. There are various surveys that serve as a tool for comparative assessment of safety culture,34 and although the results vary considerably, it is important to obtain them. In our case, the salient points were good scores for organisational learning and continuous improvement and for feedback and communication on errors.
This study has 2 limitations inherent in the study method itself, based on voluntary anonymous reporting: not all incidents were reported and some are better documented than others. Nevertheless, since we know that the importance of notification lies in its subsequent analysis,18 reporting of AEs has been shown to be the key element for obtaining information about their type, aetiology and outcome, and for instituting possible prevention strategies.24,35 On the basis of this system, by embracing the values of the culture of safety: focusing on the system, without blaming or penalising people, confidentiality, analysis of AEs by experts and use of a rapid channel of communication that is sensitive to professionals, it can be said, after 6 years, that we are on the way towards implementing this philosophy across the board in our unit and it is important not to interrupt the process and not to miss any opportunity to consolidate it.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Esqué Ruiz MT, Moretones Suñol MG, Rodríguez Miguélez JM, Parés Tercero S, Cortés Albuixech R, Varón Ramírez EM, et al. Caminando hacia una cultura de seguridad en la unidad neonatal: experiencia de 6 años. An Pediatr (Barc). 2015;83:236–243.