To estimate the effectiveness of the varicella vaccine in school outbreaks during the academic year 2009–2010.
Material and methodRetrospective cohort study in public day-care centres and/or schools in an area in the region of Murcia, Spain. The participants were all children of 1–12 years who were in the same classroom where there was an outbreak of varicella. The main measurements were the sociodemographic, clinical and vaccination data, as well as variables related to varicella disease obtained through a questionnaire self-completed by parents, and from the computerised regional immunisation registry (VACUSAN).
ResultsA total of 51 varicella outbreaks were detected, with a median of 3 cases per outbreak at both educational levels. The overall vaccination coverage was 10.7% (95% CI: 8.63–13.18), always being higher in Spanish schoolchildren versus foreign (OR: 21.21, 95% CI: 2.92–153.92, P<.001).
Discrepancies were found between the vaccine questionnaire data and vaccination programme (kappa=0.50, 95% CI: 0.43–0.58, P<.001).
According to VACUSAN, the overall attack rate was 59.7 (95% CI: 55.82–63.43) in unvaccinated and 6.5 (95% CI: 2.54–15.45) in vaccinated children. An overall effectiveness of 89.1% (95% CI: 74.55–95.35) and 100% was obtained for 1 and 2 doses of vaccine, respectively.
ConclusionsThere is a high effectiveness of varicella vaccine, emphasising that the administration of two doses of vaccine produces an adequate and optimal protection against varicella disease. A discrepancy was found between the information provided by parents and official records. Finally, there was a lower vaccination coverage in the immigrant community.
Calcular la efectividad de la vacuna de la varicela en brotes escolares durante el curso académico 2009-2010.
Material y métodoEstudio de cohortes retrospectivo realizado en guarderías y/o colegios de educación infantil o primaria públicos de un municipio de la Región de Murcia, España. Los participantes fueron el alumnado de 1 a 12 años que acudía a la misma aula donde se produjo un brote de varicela. Las mediciones principales fueron: datos sociodemográficos, antecedentes clínicos y de vacunación y variables relacionadas con la enfermedad varicelosa obtenidos a través de un cuestionario autocumplimentado por padres y/o tutores y del registro regional informatizado de vacunas (VACUSAN).
ResultadosSe detectaron 51 brotes de varicela, con una mediana de 3 casos por brote en ambos niveles educativos. La cobertura vacunal global fue del 10,7% (IC del 95%, 8,63-13,18), siendo siempre muy superior en el alumnado de nacionalidad española frente al de nacionalidad extranjera (OR = 21,21; IC del 95%, 2,92-153,92; p<0,001).
Encontramos discrepancias entre los datos vacunales del cuestionario y el programa informatizado de vacunaciones (kappa=0,50 (IC del 95%, 0,43-0,58), p<0,001).
La tasa de ataque global según VACUSAN fue de 59,7 (IC del 95%, 55,82-63,43) en no vacunados y de 6,5 (IC del 95%, 2,54-15,45) en vacunados. Obtuvimos una efectividad global del 89,1% (IC del 95%, 74,55-95,35) y 100% para una y 2 dosis de vacuna, respectivamente.
ConclusionesElevada efectividad de la vacuna de la varicela y muy especialmente en un esquema de vacunación de 2 dosis. Se han detectado discrepancias entre la información aportada por los padres y los registros informatizados regionales, así como una diferencia en la cobertura de vacunación en función de la nacionalidad.
Varicella is a worldwide infectious contagious disease, caused by the primary infection of varicella zoster virus among susceptible individuals. In the absence of vaccination, incidence is widespread, typically during childhood. It affects 86% of susceptible subjects when the virus spreads in semi-closed communities, such as day-care centres or schools, and it is essentially benign. Among newborn and adults, however, it may cause severe complications, and can even be very severe in immuno-suppressed patients.1
In 1974, Takahashi et al. in Japan developed a vaccine against varicella.2 It was initially limited to the exclusive use of immuno-suppressed patients (Europe, 1984; Japan, 1986). It was authorised for general use and systematic vaccination in Japan and South Korea in 1988 and in Sweden, Germany and the USA in 1995.
In Spain, two commercial brands have been authorised: Varilrix®3 in 1998 and Varivax®4 in 2003. Later, the Spanish Agency of Medicines and Medical Devices (Agencia Española de Medicamentos y Productos Sanitarios, AEMPS) modified the conditions for the application of both vaccines; Varilrix® in 2009 for hospital use only, and in 2013 commercial sales of the Varivax® vaccine from pharmacies were halted, and it was also restricted to hospital use only in 2014. These latest changes have resulted in a shortage of the varicella vaccine outside of hospitals.5
In 2005, the Public Health Committee of the Interterritorial Council of the Spanish National Health Service (Comisión de Salud Pública del Consejo Interterritorial del Sistema Nacional de Salud, CISNS) approved a recommendation to administer a dose of varicella vaccine to a cohort of patients aged between 10 and 14 years who had not previously had the disease nor received the vaccine.6 According to these guidelines, each autonomous community defined the vaccination procedure. In the Region of Murcia, vaccination was included in the systematic schedule in 2005–2006 for children aged 11 years, with a recommendation in favour of vaccination of susceptible individuals at high risk7 of presenting severe disease, both among children and adults, and their closest relatives. Even if this strategy does not modify the epidemiology of the disease, it may reduce incidence at ages in which complications can be more dangerous.
According to the literature, effectiveness of the vaccine ranges between 72% and 100%, depending on the type of study, vaccination coverage, and the number of administered vaccine doses.8 There are few studies in our country about the effectiveness of the vaccine, and those that are published9,10 have been conducted only in single outbreaks of varicella, with a small number of cases, and estimating the effectiveness of the vaccine with wide confidence intervals. Given the epidemiological importance of varicella and the scarcity of valid data on its effectiveness in school outbreaks in our country, we undertook this study with the objective of calculating the effectiveness of the varicella vaccine in the context of several outbreaks in educational centres during the 2009–2010 academic year, and to describe the socio-demographic characteristics of schoolchildren involved in the programme.
MethodType of studyRetrospective cohort study.
Study populationThe study was conducted during the 2009–2010 academic year in Totana, a municipality belonging to the III Health Area in the Region of Murcia, with a population of 29,211, with a total of 15.3% of the population under 13 years, according to data from the National Statistics Institute for the year 2009.
The dependent variable under study was presentation of varicella. Following the clinical criteria set by the National Network of Epidemiological Surveillance in the CISNS in 2001, a varicella patient was defined as one who presented a sudden rash or maculopapular vesicular exanthema, in the absence of any other apparent cause.
The independent variable analysed was having received the varicella vaccine, considering schoolchildren with at least one dose of the vaccine as exposed.
A varicella outbreak was defined as the existence of more than one person with varicella in a period of 3 weeks in the same classroom.
Children born in Spain, but with parents of a nationality other than Spanish, were considered foreign schoolchildren.
Those cases where, in spite of the vaccine, the disease was present 42 days after vaccination were defined as breakthrough varicella. These cases tend to present milder symptoms of the disease, although they are still infectious.
All schoolchildren attending day-care centres (under 3 years), and in nursery schools and primary education schools (under 13 years), all schoolchildren in the same classroom where an outbreak occurred were included in the study.
The population attending private day-care centres, subjects who had presented varicella before the school year under study, and patients presenting with varicella within the first 42 days after vaccination according to the computerised regional immunisation registry (VACUSAN) were excluded from the study.
Sample size and selectionAll schoolchildren involved in outbreaks during the study period were selected.
Procedure and data collectionThe status of disease was determined by doctors’ reports obtained from the Notifiable Disease Surveillance System. The existence of an outbreak in the classrooms was verified through an active nominal search of patients using the OMI statistics program. Once a student with varicella was identified, the case was located in the corresponding educational centre by consulting the nominal database provided by the Teaching Council of the Region of Murcia. At the end of the year, in all classrooms where a varicella outbreak was detected, teachers gave all students, whether patients or not, a questionnaire to be completed by their parents or guardians (Appendix 1).
A questionnaire was used as a data-collection tool, gathering socio-demographic variables (age, sex and nationality of the parents), clinical (chronic diseases and treatment) and vaccination history, clinical variables related to varicella disease (prior occurrence of the disease and age at onset of varicella). The questionnaire had a structure similar to Gould et al.11 and Spackova et al.,12 with closed questions and dichotomic answers, as well as semi-closed questions to expand on the information supplied. A pilot test was conducted first to adjust the questionnaire to our context.
The information was supplemented with a review of the medical records of primary care patients and of the regional vaccination registry. Data was uploaded independently by 2 professionals in order to minimise errors.
Statistical analysisData was analysed with the statistical package SPSS 21. Qualitative variables were shown as frequencies and percentages. For symmetrical quantitative variables, the median and standard deviations (SD) were calculated, and in asymmetrical variables, the median and interquartile range (P25-P75). The comparison of proportions was made by means of the chi-square test (χ2), and, if the variable was categorical ordinal, the χ2 of linear trend (χ2LT). Student's t and Mann–Whitney U tests, and the variance analysis were used for numeric variables. The odds ratio (OR) was calculated as measurement of magnitude, with confidence intervals (CI) of 95%. The descriptive aspect of logistic regression was used for the trend analysis and the kappa index to assess the concordance between variables. A significance level of 5% (p≤0.05) was set.
Effectiveness of the vaccineThe disease attack rate of vaccinated (ARV) vs. unvaccinated (ARU) subjects was calculated. The effectiveness of the vaccine was calculated according to the Greenwood–Yule13 formula: (ARU−ARV)/ARU*100. Schoolchildren who had previously experienced varicella were excluded from this calculation.
Ethical considerationsThe study was approved by the Clinical Research Ethics Committee of the University Hospital Virgen de la Arrixaca.
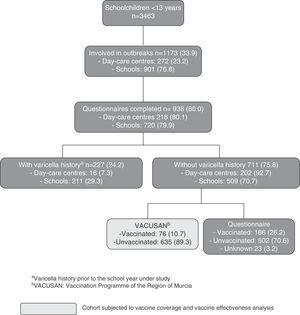
ResultsThe school population under 13 years comprised 3463 students (Fig. 1), of which 52.6% (n=1823) were boys. During the study period, 51 outbreaks of varicella were detected (Table 1), with a significantly higher proportion occurring in day-care centres and nursery schools than among schoolchildren in primary education.
Distribution of all schoolchildren by educational level.
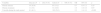
| Educational level | Classrooms | Total schoolchildren | Mean age (SD), years | Outbreak classrooms (%) | OR | 95% CI | p | Mean schoolchildren per outbreak (SD) |
|---|---|---|---|---|---|---|---|---|
| Daycare | 18 | 272 | 2.53 (0.5) | 13 (72.2) | 22.2 | 6.4–77.0 | <0.001 | 3.00 (1.2) |
| Nursery school | 47 | 1.123 | 4.98 (0.9) | 29 (61.7) | 13.8 | 5.6–34.1 | <0.001 | 5.52 (2.6) |
| Primary | 86 | 2.068 | 9.35 (1.8) | 9 (10.5) | 1.0 | 3.67 (1.9) | ||
| Total | 151 | 3.463 | 7.39 (2.9) | 51 (33.8) | 4.54 (2.5) |
SD: standard deviation; CI: confidence interval; OR: odds ratio.
The questionnaire was administered to a total of 1173 schoolchildren, all of them related to the detected varicella outbreaks, of whom 76.8% (n=901) attended schools. The global response rate was 80.0% (n=938). The socio-demographic characteristics of those who completed the same are shown in Table 2.
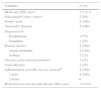
Socio-demographic data by educational level of schoolchildren who completed the questionnaire (N=938).
| Variables | Daycare, N (%) | School, N (%) | OR | 95% CI | p |
|---|---|---|---|---|---|
| Completed questionnaire | 218 (80.1) | 720 (79.9) | 1.0 | 0.7–1.4 | 0.70 |
| Questionnaire respondent | |||||
| Mother | 197 (90.4) | 647 (89.9) | 0.9 | 0.6–1.6 | 0.93 |
| Father | 21 (9.6) | 73 (10.1) | |||
| Gender | |||||
| Boy | 123 (56.4) | 372 (51.7) | 0.8 | 0.6–1.1 | 0.25 |
| Girl | 95 (43.6) | 348 (48.3) | |||
| Median age years (IQR) | 2.6 (2.1–3.0) | 5.3 (4.2–6.6) | <0.001a | ||
| Nationality of father | |||||
| Spanish | 203 (93.1) | 548 (76.1) | 4.2 | 2.4–7.4 | <0.001 |
| Foreign | 15 (6.9) | 172 (23.9) | |||
| History of varicella | 16 (7.3) | 211 (29.3) | 5.2 | 3.1–8.9 | <0.001 |
CI: confidence interval; IQR: interquartile range; OR: odds ratio.
Once the questionnaires were analysed, it was found that 24.2% (n=227) had had varicella prior to this school year. These respondents were excluded and data from the remaining 711 students was analysed.
Table 3 shows vaccine status stratified according to the educational level. According to VACUSAN, the vaccination coverage of schoolchildren attending day-care centres (15.3%) was higher than that of schools (8.8%), giving a global vaccination coverage of 10.7% (n=76). Furthermore, it was shown that the coverage of Spanish nationals was always far higher than that of foreign nationals; the difference was significant (OR=21.21; 95% CI: 2.92–153.92; p<0.001). As for the varicella vaccine data, we found discrepancies between the vaccine questionnaire data and the regional vaccination programme (kappa=0.50 [95% CI: 0.43–0.58]; p<0.001), with a global concordance of 84.0%.
Vaccine status by educational level (N=711).
| Vaccination | Daycare, N (%) (n=202) | School, N (%) (n=509) | OR | 95% CI | p |
|---|---|---|---|---|---|
| According to VACUSAN | |||||
| Vaccinated | 31 (15.3) | 45 (8.8) | 0.5 | 0.3–0.9 | 0.02 |
| Nationality | |||||
| Spanish | 30 (14.9) | 45 (8.8) | 21.2 | 2.9–153.9 | <0.001 |
| Not Spanish | 1 (0.5) | 0 (0) | |||
| Varicella coverage | |||||
| 1 dose | 28 (13.9) | 34 (6.7) | 3.0 | 0.8–11.9 | 0.19 |
| 2 doses | 3 (1.5) | 11 (2.2) | |||
| Mean age (SD), years | |||||
| 1 dose | 1.5 (0.4) | 1.9 (1.0) | <0.001a | ||
| 2 doses | 2.1 (0.4) | 4.3 (1.2) | 0.7 | 0.1–3.5 | 0.001a |
| Mean age V/D (SD), years | 1.3 (0.7) | 1.6 (0.4) | 0.71 | ||
| Vaccination centre | |||||
| Public | 28 (13.9) | 42 (8.3) | 0.97 | ||
| Private | 3 (1.5) | 3 (0.6) | |||
| Commercial brandb | |||||
| Varivax® | 31 (100) | 41 (91.1) | 1.1 | 1.0–1.2 | 0.24 |
| Varilrix® | 0 (0) | 4 (8.9) | |||
| According to survey | |||||
| Vaccinated | 61 (30.2) | 125 (24.6) | 0.8 | 0.5–1.1 | 0.17 |
| Varicella coverage | |||||
| 1 dose | 55 (27.2) | 93 (18.3) | 3.0 | 1.2–7.6 | 0.03 |
| 2 doses | 6 (3.0) | 30 (5.9) | |||
CI: confidence interval; SD: standard deviation; OR: odds ratio; V/D: vaccine/disease.
The disease attack and effectiveness rates were analysed according to data from the regional vaccination programme (Table 4). The disease attack rate of unvaccinated students was higher in schools, although no significant differences were found (OR=3.80; 95% CI: 0.53–27.38; p=0.16), whereas among vaccinated students it was similar at both educational levels.
Rates of disease attack and effectiveness of the vaccine by educational level.a
| Daycare (95% CI) | Schools (95% CI) | Global (95% CI) | |
|---|---|---|---|
| Attack rate of unvaccinated students | 46.20 (38.89–53.67) | 64.66 (60.20–68.87) | 59.69 (55.82–63.43) |
| Attack rate of vaccinated students | 6.45 (1.79–20.72) | 4.44 (1.23–14.83) | 5.26 (2.07–12.77) |
| 1 dose | 7.14 (1.98–22.65) | 5.88 (1.63–19.09) | 6.45 (2.54–15.45) |
| 2 doses | 0 (0–56.15) | 0 (0–25.88) | 0 (0–21.53) |
| Effectiveness | |||
| 1 dose | 84.54 (40.64–95.97) | 86.74 (60.80–95.52) | 89.12 (74.55–95.35) |
| 2 doses | 100 | 100 | 100 |
CI: confidence interval.
We observed an association between presenting the disease and not being vaccinated (OR=16.7; 95% CI: 8.3–33.3; p<0.001), showing that having the disease or not was influenced by the number of doses administered (χ2TL=111.61, p<0.001). Thus, the effectiveness of the vaccine in schoolchildren who had one dose was 89.12% (95% CI: 74.55–95.35) and 100% in those who had 2 doses, as shown in Table 4.
When we analysed the clinical history, we observed that 53.9% (n=383) had varicella during the school year under study (Table 5).
Clinical history and varicella status by educational level (N=711).
| Variables | Daycare (N=202) N (%) | School (N=509) N (%) | OR | 95% CI | p |
|---|---|---|---|---|---|
| Chronic disease | 34 (16.8) | 67 (13.2) | 0.7 | 0.5–1.2 | 0.25 |
| Chronic treatment | 11 (5.4) | 51 (10.0) | 1.9 | 1.0–3.8 | 0.07 |
| Varicella during the study period | 81 (40.1) | 302 (59.3) | 2.2 | 1.6–3.0 | <0.001 |
CI: confidence interval; OR: odds ratio.
Notably, 4 students had modified varicella in spite of having received one vaccine dose against varicella. The characteristics of the subjects are shown in Table 6.
Description of the 4 cases of modified varicella.a
| Variables | N (%) |
|---|---|
| Mean age (SD), years | 3.7 (1.1) |
| Educational centre: school | 2 (50) |
| Gender male | 4 (100) |
| Nationality Spanish | 4 (100) |
| Diagnosed by | |
| Paediatrician | 3 (75) |
| Guardians | 1 (25) |
| Disease history | 4 (100) |
| Atopic dermatitis | 4 (100) |
| Asthma | 1 (25) |
| Chronic corticosteroid treatment | 1 (25) |
| Food allergies | 1 (25) |
| Administrated varicella vaccine Varivax® | 4 (100) |
| 1 dose | 4 (100) |
| 2 doses | 0 |
| Mean between vaccine and disease (SD), years | 1.5 (0.5) |
SD: standard deviation.
This is the first study conducted in the Region of Murcia on varicella outbreaks in schoolchildren under 13 years. All 51 outbreaks detected were associated with lower ages, mainly affecting day-care centres and nursery school classrooms, confirming that varicella outbreaks in our study affected mainly classrooms of children under 6 years, since at these ages they are more susceptible as they have not previously been exposed to the virus.14
Spain has implemented 2 vaccination strategies against varicella. Even though both recommend vaccination in susceptible teenagers, only Navarra, Ceuta and Melilla include vaccination during infancy in the vaccination schedule. This recommendation was also made in the Community of Madrid until 31 December, 2013. In studies15,16 conducted in these communities, with coverage above 90%, a dramatic drop in incidence of the disease has been confirmed, both among vaccinated and unvaccinated students, possibly due to the group immunity conferred by the vaccine. The recent report14 by the National Epidemiology Centre confirms the high vaccination coverage both in Navarra (96.1%) and in Madrid (91.1%) in 2009. However, in the Community of Valencia and in Murcia, where vaccination is not included during the first year, coverage was 39% and 22.9%, respectively, for the same year. This universal vaccination strategy in childhood has reduced incidence of varicella by 64% compared to pre-vaccination data, but only by 16% in communities that have not implemented this program.
An analysis of the disease attack rates in unvaccinated students showed that these were higher in children attending school. Although these rates were comparable to those reported by Arnedo et al.9 and Galil et al.,17 studies in other countries such as Turkey,18 Italy19 and the United States.20 Notably, the study published by Lopez et al.21 in a population in Arkansas reported a rate of 100%.
These authors obtained an effectiveness of 82%, showing that a vaccine coverage of 99% with a single dose was not enough to prevent school outbreaks, a finding echoed in an earlier study.22 Furthermore, our effectiveness values were homogeneous both in relation to earlier research and to other studies,11,12,23 and very superior to the 44% observed in a day-care centre in the USA17 and the 20% in 8 day-care centres in Israel.24 It is important to note that the strong point of our study lies in the fact that the effectiveness calculation of the vaccine has been made based on schoolchildren with confirmed presence of varicella outbreaks, ensuring, therefore, true exposure to the varicella virus.
Another notable finding on analysing socio-demographic data is that nearly a quarter of schoolchildren were foreigners, with most being of Ecuatorian origin, due to the impact of the migration phenomenon in the municipality and the characteristics of this group in our health area.25 Lower vaccine coverage against varicella was detected in this population segment, as recorded in the study conducted in Barcelona,26 where immigrant status is a predictive factor in the delay in receiving and/or completing a program of systemic vaccination. This inequality may be exacerbated in vaccinations not subsidised by the public health system, as is the case of the varicella vaccine in our region in children under 11 years.
As for the age of administration of the first dose in vaccinated children, we observed a major discrepancy with regard to the recommendations suggested by the vaccine schedule of the Region of Murcia. This shows that vaccination has been administered based on criteria that differ notably from those defined by the regional health authorities, possibly based on the guidelines of the Spanish Paediatric Association.27
Like Lai et al.,28 we analysed the correlation between the self-administered questionnaire and the vaccination programme. Although the association was weak, we achieved a moderate level of agreement. We further note that this type of analysis was not conducted in other articles we reviewed, in spite of its relevancy, since we found a higher rate of positive responses to having received the vaccine in the information provided by the guardians. This finding was further evidenced in the study of Jiménez-García et al.29 For this reason the effectiveness of the varicella vaccine was based on official records, since they have proven to be more reliable.
In the USA during varicella outbreaks, the public health services vaccinate roommates susceptible to developing the varicella disease. In our country, where the vaccine is not included in the first infancy schedule, there is no such recommendation. This encourages the natural spread of the virus and does not break its epidemiologic chain, reducing the number of susceptible subjects in adult age, when varicella presents a greater number of complications.
Absence of data from private day-care centres was a limitation on the study, since this population might have different socio-demographic and epidemiologic characteristics and vaccine status. Due to the self-administered nature of questionnaire completed at the end of the course, there may be bias of memory, as well as a higher rate of positive answers by guardians with regard to vaccination status, as was shown in the concordance analysis. This potential under-recording of vaccine doses in the population database (VACUSAN) might underestimate the effectiveness of the vaccine in this population. The study has brought to light discrepancies between information in official records and that supplied by parents, leaving the quality of these records open to question. This is an interesting topic for future research. Another notable limitation is the varicella prognosis applied in this study, which only took into consideration clinical criteria for diagnosis, without including confirmation lab tests for any student. For this reason, the effectiveness of the vaccine might be overestimated if there was modified varicella that was not clinically relevant.
As a general conclusion, the high effectiveness of the varicella vaccine is notable, and even more so in a 2-dose vaccination scheme, resulting in optimum protection against the disease. Discrepancies have also been detected between information supplied by parents and regional electronic records, as well as a difference in the vaccination coverage based on nationality.
Authors’ contributionAll the authors have intellectually contributed in this work, meeting the authorship conditions, and have approved the final version of the same. This work has not been submitted to any meeting, congress or symposium.
Conflict of interestThe authors state there is no conflict of interest.
To José Antonio Navarro Alonso and Pedro José Bernal, for the interest shown in this project. To the Teaching Council of the Region of Murcia, that facilitated this research project, and to all the education personnel who collaborated in the application of the questionnaire at school centres.
Particularly, we would like to thank the parents who completed the questionnaire; this work would not have been possible without them.
Please cite this article as: Romera-Guirado FJ, Molina-Salas Y, Pérez-Martín JJ, Ruzafa-Martínez M. Efectividad de la vacuna de la varicela en el contexto de brotes escolares en una zona semiurbana. An Pediatr (Barc). 2016;84:30–38.