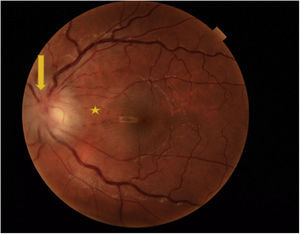
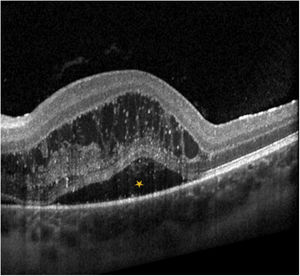
A patient aged 13 years presented with fever, unilateral colour discrimination deficits and impaired vision. The findings of blood tests and the head CT were normal. The fundoscopic examination revealed oedema in the optic disc and peripapillary retina (Fig. 1) and the optic coherence tomography scan evinced macular oedema (Fig. 2), findings compatible con neuroretinitis. The diagnosis was confirmed by serology (positive for Bartonella henselae).
Cats are the main reservoir of B. henselae, which causes cat scratch disease. The disease typically manifests in the form of self-limiting lymphadenopathy, but it can also have a systemic presentation, for instance, disease manifesting with ocular involvement.1
Neuroretinitis secondary to B. henselae infection is rare. Its characteristic features are unilateral loss of visual acuity and visualization of optic disc oedema and exudates around the macula (macular star) in the fundoscopic examination.1–3 The macular star usually develops 1–4 weeks from onset and persists for several months (Fig. 3).2 Treatment consists of prolonged dual therapy (doxycycline and rifampicin). The use of steroid therapy remains controversial, although there is evidence suggesting that it may improve fundoscopic abnormality and visual acuity outcomes.1,3
The differential diagnosis of unilateral vision loss with optic disc oedema must include optic neuritis, which may develop after an infection or vaccination or in the context of acquired demyelinating disease.1