Parental obesity is a risk factor for childhood obesity. The aim of this study was to determine if parental obesity influences the adherence and success of obesity treatment in a hospital paediatric endocrinology clinic.
Material and methodsAn analytical, prospective, longitudinal study was conducted on obese children aged 4–14. An initial body mass index (BMI) was obtained, and again at 6 months after receiving health, hygiene and dietary recommendations. Success was considered as a decrease of 0.5 in the BMI z-score, and adherence to attending the 6-month review. Parental BMI was determined to identify overweight. The χ2 test was used for qualitative variables and the T-Student test for quantitative (significance, P<.05) variables.
ResultsThe study included 100 children (52 male), 9.9±2.7 years old, BMI 28.1±4.5kg/m2 and BMI z-score 3.11±0.98 (85% had a BMI z-score>3). More than half (59%) of the children had one or both parents obese (41 fathers and 37 mothers were obese). Treatment was not adhered to by 25 children. Adherence was worse if both parents were obese, OR 3.65 (1.3–10.5) (P≤.01), and adherence was better if the mother was not obese, although the father was (P=.01). The treatment had significant success in 40 patients. If the mother was the only obese one in the family, the possibility of treatment failure was greater, OR 5.6 (1.4–22.4) (P<.01).
ConclusionsA high percentage of children with severe obesity have obese parents. The mother has an important influence on adherence and response to treatment for the severely obese child.
El objetivo del estudio es conocer si tener padres obesos influye en la adherencia y el éxito del tratamiento frente a la obesidad en la consulta de endocrinología infantil de un hospital.
Material y métodosEstudio analítico, prospectivo y longitudinal en obesos de 4–14 años. En ellos se determinó el IMC inicial y 6 meses después de que recibieran pautas higiénico-dietéticas saludables. Se consideró éxito significativo la disminución de 0,5 DE del IMC y adherencia que los pacientes acudieran a la revisión semestral. Se calculó el IMC de los padres para identificar a los obesos. Se utilizó el test de la χ2 para comparar las variables cualitativas y el test de la t de Student para las variables cuantitativas (significativo: p<0,05).
ResultadosCien niños (52 varones), edad media±DE: 9,9±2,7 años, IMC 28,1±4,5kg/m2 y z-score del IMC 3,11±0,98 (el 85% tenía un z-score del IMC>3). Eran obesos 41 padres y 38 madres (el 59% tenía uno o los 2 padres obesos). No se adhirieron al tratamiento 25. La adherencia era peor si los 2 padres eran obesos, OR 3,65 (1,3–10,5) (p=0,01) y era mejor si la madre no era obesa, aunque el padre lo fuera (p=0,01). El tratamiento tuvo éxito significativo en 40 pacientes. Si la madre era la única obesa en la familia la posibilidad de no tener éxito era mayor, OR 5,6 (1,4–22,4) (p<0,01).
ConclusionesUn alto porcentaje de niños con obesidad severa tienen padres obesos. La madre tiene gran influencia en la adherencia y respuesta al tratamiento frente a la obesidad del hijo muy obeso.
Childhood obesity is a public health problem in developed countries. The World Health Organisation (WHO) has called obesity the XXI century epidemic due to the proportions it has acquired and its impact on morbidity, mortality, quality of life and health care costs.1,2 Europe has a surveillance system that has alerted us to the high prevalence of childhood obesity in countries in southern Europe.3 Spain ranks third in Europe, with a 19.1% prevalence of childhood obesity and a 26.1% prevalence of childhood overweight, according to the Estudio de Alimentación, Actividad física, Desarrollo Infantil y Obesidad (Study on Nutrition, Physical Activity, Childhood Development and Obesity [ALADINO]) conducted in 2011.4
Childhood obesity is a multifactorial condition. The literature has described many risk factors involved, including parental obesity and sociocultural level. A study conducted in Sweden by Moraeus et al.5 addressed the importance of the association between parental obesity and future obesity in their children. The study conducted in Spain by Santiago et al.6 also referred to the importance of parental obesity, which was the best predictor of childhood overweight in both sexes. Rodriguez et al.7 reported that a high percentage of parents in Spain do not correctly assess the weight status of their overweight children, especially at earlier ages. This inadequate perception by overweight parents may also be a risk factor for childhood obesity. Several studies have concluded that parents influence the dietary behaviours of their children concerning food preferences and the type, amount, and quality of consumed foods.8
It seems evident that there is a significant relationship between obesity in parents and obesity in their children. However, few studies have assessed whether obesity in the parents once children are already obese can influence the children's response and adherence to obesity treatment. It is known that mothers are mainly responsible for passing on healthy dietary habits to their children,9,10 but it is not known whether the response to obesity treatment varies depending on which of the parents is obese. There is also some degree of controversy as to whether parents influence the nutritional status of their children throughout their entire development, or whether their influence reaches only as far as 10 years of age or the beginning of puberty.11 Knowing this would help us implement more effective therapeutic strategies.
The aim of this study was to learn whether having obese parents influenced the response and adherence to treatment of obese children, and to analyse the response to lifestyle and dietary recommendations given to the population under study at the paediatric endocrinology clinic.
Materials and methodsWe conducted a prospective, longitudinal analytical study. We recruited children and adolescents aged 4–14 years referred by their paediatrician to the paediatric endocrinology clinic of a tertiary hospital between November 2010 and November 2012 for obesity treatment. The children's weight (kg), height (cm) and waist circumference (cm) were measured at the clinic, followed by calculation of their body mass index (BMI, kg/m2) and z-scores for weight, height, BMI and waist circumference for their sex and age (charts of the 2010 Spanish study by Carrascosa for weight, height and BMI; charts of the cross-sectional 2011 Fundación Orbegozo study for waist circumference).12,13 The degree of pubertal development was assessed during the physical examination (prepubertal: Tanner stage 1, and pubertal: Tanner stage>1).
Patients were included in the study as they were referred to the clinic by their paediatricians, and the sole inclusion criterion was that they have a BMI z-score above 2 for their age and sex. We excluded patients with neuropsychological disorders, such as neurodevelopmental delay or autism, as these disorders would influence response to lifestyle and dietary interventions, and patients that received a diagnosis of clinical hypothyroidism or hypercortisolism based on the initial laboratory tests.
During the first visit, lifestyle and dietary recommendations were given to both the parents and the child (Appendix 1), recommending daily physical activity and a diet based on on-demand and light-calorie foods according to the classification of foods presented in Appendix 2.
Thereafter, patients came for medical checkups at the paediatric endocrinology clinic of the hospital. The first checkup was scheduled at one month, and subsequent checkups every one to two months, during which the lifestyle and dietary recommendations and the advice to perform physical activity for 1h a day were reinforced. At six months after the first visit, patients were assessed once more, measuring their weight, height, BMI and waist circumference and recalculating their z-scores for all parameters. We defined success as a decrease of 0.5 or more in the BMI z-score, and adherence to treatment as showing up to the six-month checkup.
During the first checkup, the weight and height of both parents were measured, and their BMI calculated (kg/m2). Based on their BMI, parents were classified into: underweight (<18.5kg/m2), normal weight (18.5–24.9kg/m2), class I overweight (25.0–26.9kg/m2) or class II overweight (27.0–29.9kg/m2), moderate obesity (30.0–34.9kg/m2), severe obesity (35.0–39.9kg/m2), morbid obesity (40.0–49.9kg/m2) and extreme obesity (>50kg/m2), following the 2000 classification scheme of the Sociedad Española para el Estudio de la Obesidad (SEEDO).14 In order to determine the association between the children's response to treatment and parental weight, we divided parents into obese and not obese.
We performed the statistical analysis of the results with the statistical package SPSS V.19. We have expressed qualitative variables as mean±standard deviation (SD) and compared them with the Student t test verifying that they followed a normal distribution by means of the Kolmogorov–Smirnov test. We compared categorical variables with the χ2 test. We set a confidence interval of 95% (significance, P≤.05). We assessed risk by calculating the odds ratio (OR).
The parents of the patients were informed and asked to agree to take part in the study when it was observed that the patients met the inclusion criteria.
ResultsWe studied a total of 100 obese children, 47 girls and 53 boys, with a mean age of 9.91±2.73 years. In terms of pubertal development, there were 25 prepubertal and 28 pubertal girls, and 31 prepubertal and 16 pubertal boys.
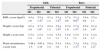
Anthropometric characteristics of the sampleFig. 1 presents the degree of obesity of the sample on the 2 occassions it was assessed (M1 and M2), which was determined on the basis of the BMI z-score. A high percentage of children (82%) had high-degree obesity at the beginning of the study (BMI z-score≥3).
Degree of obesity of the sample based on the BMI z-score at the time of the initial measurement (M1) and the measurement at six-month checkup (M2), applying the 2010 cross-sectional study charts. Source: Carrascosa et al.12
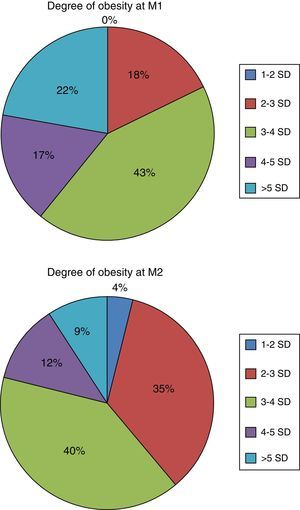
Table 1 summarises the anthropometric characteristics (height, weight and BMI z-score) of the patients at the time of the first measurement (M1) and the second measurement (M2). For each group, we compared the data obtained at M1 and M2 by means of the Student t test for paired samples, and found statistically significant differences, with the group of pubertal boys being the only one in which there was no statistically significant difference between the BMI z-scores obtained during M1 and M2 (Table 1).
Anthropometric measurements of the sample (mean±SD) at the time of measurement 1 (M1) and measurement 2 (M2) by patient group.
| Girls | Boys | |||||||
|---|---|---|---|---|---|---|---|---|
| Prepubertal | Pubertal | Prepubertal | Pubertal | |||||
| M1 | M2 | M1 | M2 | M1 | M2 | M1 | M2 | |
| BMI z-score (kg/m2) | 4.4±1.6 | 3.5±1.4** | 4.1±1.2 | 3.5±1.4** | 3.7±0.9 | 3.1±0.9** | 3.9±0.8 | 3.5±1.1 |
| Weight z-score (kg) | 4.2±1.6 | 3.7±1.9* | 4.4±1.3 | 3.8±1.5** | 4.3±1.6 | 3.7±1.5** | 4.6±1.6 | 4.1±1.8* |
| Height z-score (cm) | 1.5±1.3 | 1.5±1.4 | 1.4±1.1 | 1.5±1.1 | 1.4±1.1 | 1.5±1.1 | 1.3±1.4 | 1.2±1.7 |
| Waist circumference z-score (cm) | 5.48±1.5 | 4.95±1.18 | 5.8±1.4 | 5.5±1.8 | 3.8±1.1 | 3.3±1.3** | 3.8±1.1 | 3.2±1.2* |
Student t test for dependent means comparing M1 and M2 in each group.
Based on the SEEDO classification, 27% of mothers had normal weights, 36% were class I or class II overweight, and 37% were obese to some degree. When we compared the mean BMIs of the mothers with the Student t test we found statistically significant differences (P<.05) between the mothers of pubertal children and the mothers of prepubertal children (Table 2). Of the mothers of pubertal children, 46% were obese and up to 13% were morbidly obese; while only 28% of the mothers of prepubertal children had class I or II obesity, and none had morbid obesity.
Anthropometric measurements of the mothers and fathers of the patients (mean±SD) by patient group; Student t test for independent samples.
| Girls | Boys | |||
|---|---|---|---|---|
| Prepubertal | Pubertal | Prepubertal | Pubertal | |
| Maternal weight (kg) | 76.1±12.7 | 73.9±15 | 72.4±13.4 | 80±13.3 |
| Maternal height (m) | 1.6±0.1 | 1.6±0.1 | 1.6±0.1 | 1.6±0.1 |
| Paternal weight (kg) | 87.9±16.4 | 88.6±15.1 | 93.6±22.2 | 87±14.9 |
| Paternal height (m) | 1.8±0.1 | 1.7±0.1 | 1.7±0.1 | 1.7±0.1 |
| Paternal BMI (kg/m2) | 28.6±4.5 | 30.9±5.7 | 30.6±6.3 | 29.5±3.8 |
| Maternal BMI (kg/m2) | 28.7±4.8 | 28.6±5.6 | 27.7±5.8 | 31.7±6.6* |
Of all fathers, 12% had normal weight, 45% some degree of overweight, and up to 41% some degree of obesity, with 1% being morbidly obese and 1% extremely obese. We found no significant differences between groups in the comparison of the paternal anthropometric data (Table 2).
Both parents were obese in 19 patients, only the mother was obese in 18, only the father was obese in 22, and in 41 patients neither parent was obese.
Adherence to recommendationsTwenty-five patients did not show for the six-month visit when the second measurements were taken. Sixty-four percent of these patients (16/25) had one or two obese parents; only the mother was obese in four, only the father was obese in three, and both parents were obese in nine. Table 3 shows the data for the two groups of patients, those that adhered to treatment and those that did not. The mothers of non-adherent patients had higher BMIs (P<.05). When we compared the fathers, we found no statistically significant differences.
Data for the adherent and non-adherent patient groups described as mean±SD.
| Non-adherent | Adherent | |
|---|---|---|
| Age (years) | 10.8±2.6 | 9.6±2.7 |
| Maternal weight (kg) | 78.7±18.9 | 73.7±11.2 |
| Maternal height (m) | 1.6±0.1 | 1.6±0.1 |
| Maternal BMI (kg/m2) | 30.8±5.4* | 28.2±4.9 |
| Paternal weight (kg) | 93.7±23.1 | 88.4±15.6 |
| Paternal height (m) | 1.7±0.1 | 1.7±0.1 |
| Paternal BMI (kg/m2) | 29.1±11.2 | 28.6±6.7 |
| Patient's BMI (kg/m2) | 29.7±3.5 | 27.6±4.6 |
| Patient's BMI z-score | 4.3±1.4 | 4±1.1 |
| Patient's height z-score | 1±1.1 | 1.3±1.2 |
| Patient's weight z-score | 4.4±1.2 | 4.3±1.6 |
Student's t test.
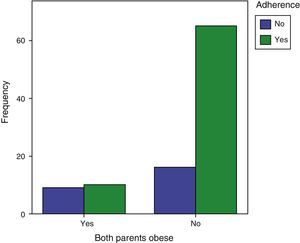
When we compared the adherent and non-adherent groups in terms of having an obese mother, father or both by means of the χ2 test, we found that when the mother was not obese, even if the father was obese, adherence was higher than when both parents were obese (P=.013). We also observed that adherence to treatment was worse when both parents were obese than when they were not (P=.012). When both parents were obese, children were 3.65 times more likely (CI, 1.3–10.5) to not adhere to recommendations than if they were not (Fig. 2).
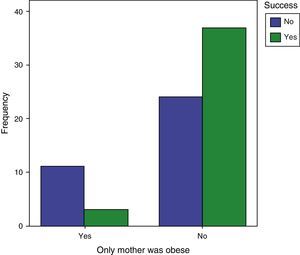
Treatment successAfter six months of follow-up, the BMI z-scores of 23 patients had decreased by more than 1, the z-scores of 17 by 0.5–1, and those of 20 patients decreased by 0.1–0.5, while in 11 the z-scores increased by 0.5 or less, and in 4 they increased by more than 0.5. Thus, 40% of the patients included at the beginning of the study were significantly successful following the lifestyle and dietary recommendations.
Of the group of 40 patients that were significantly successful, 19 (47.5%) did not have an obese parent, and in 3 (7.5%) only the mother was obese. When we analysed patient success based on the presence of parental obesity by means of the χ2 test, we found that the probability of not succeeding was significantly higher if the mother was the only obese parent (OR, 5.65 [1.4–22.4]; P=.008) (Fig. 3).
DiscussionThe percentage of children in this study that adhered to the recommendations may seem low, as only 75% showed at the six-month checkup. In the study by Feliu et al.15 adherence reached 78.2% at 12 months, and there are even studies in which losses to follow-up amount to only 9% and 7% at 12 months,17 although in these studies the checkups were conducted at home or in the school. In our study, the checkups were performed in a tertiary hospital to which patients needed to travel, sometimes from towns more than 1h away and through mountainous terrain. The time available for the first visit was 20min, and subsequent visits lasted only 5min. Some studies have indicated that durations of less than 15min per visit could suffice for motivational modalities of obesity treatment.18 At any rate, assessing the delivery of care with the means and time that are actually available in the endocrinology clinic of a public tertiary hospital can be useful for the purposes of considering possible changes in treatment strategies.
In this study, we found a success percentage of 40%, which was lower than the percentages found by other studies that defined success as a z-score decrease of any size.15 If our study had considered any decreases in z-scores a success, the success percentage would have reached 60% in patients that started the treatment, and 80% in patients that completed it, similar to the results of other studies that applied broader measures of treatment success. There is no consensus on the time that is needed to assess the response to obesity treatment, but it should be of at least six months.19 Some studies have analysed periods of up to 12 and 24 months,16,17 so we cannot compare the data. However, initial response is a good prognostic factor, and patients that do not show an initial response are unlikely to show one at a later time.
When it came to the family history, a high percentage of patients had at least one obese parent. The average BMI of the mothers ranged between 27.7kg/m2 in mothers of prepubertal children and 31.7kg/m2 in mothers of pubertal children, which were within the overweight and obesity ranges, respectively. The average BMI of the fathers ranged from 28.6kg/m2 to 30.9kg/m2, which also corresponded to the overweight and obesity ranges. This was consistent with the findings of Feliu Rovira et al.15 It seems clear that a high proportion of children that are very obese have obese parents, demonstrating that the family plays an essential role in the prevention of childhood obesity. This association between obesity in children and obesity in their parents can be explained not only by environmental or behavioural factors (as they share dietary and physical activity habits), but also by genetic factors as well.20
When we assessed the response to the lifestyle and dietary recommendations in relation to whether the parents were or were not obese, the importance of the mother's role stood out, for when the mother was obese, irrespective of the father being obese or not, the response to treatment was much worse. This may be related to the fact that mothers are mainly responsible for dietary habits. If the mother is obese, her dietary habits may not be healthy, and she may find it difficult to change her own diet, with fathers probably having a lesser involvement in their children's dietary habits. Other studies have shown that the immediate family, and especially mothers, has a significant influence on the child's dietary behaviours,21–23 and our study corroborates the role of the mother.
Thus, it seems that it is very important that parents become more involved in their children's diet, and to try to change the dietary habits of the mother if she is obese, for otherwise, as our study suggests, the outcomes of their children will be worse. The findings of other studies have evinced that the treatment of childhood obesity and overweight must be firmly founded on the development of healthy habits and the promotion of physical activity, and that the awareness and level of involvement of the family are crucial factors in the development of healthy lifestyles by the young.24
Another noteworthy finding is that the mother plays a key role in following through with checkups at the paediatrician's office, and therefore in adherence to treatment. The mothers of children that stopped showing for checkups were more obese. It may be that obese mothers are less likely to adhere to treatment because they do not consider obesity a health problem. Perhaps it would be convenient to implement treatment strategies that involve the mother as well as the child. An improvement in BMI in children is probably dependent on succeeding in improving the BMI in mothers, as noted by Limbers et al.25 and Nyberg et al.26 Unfortunately, our study did not collect the BMI of both parents after the period during which the child was followed up. These data would have provided information as to whether there had been a change in lifestyle and dietary habits in the family as a whole.
In our study, the response to lifestyle and dietary recommendations was worse among pubertal children. This may be related to the fact that the mothers of pubertal children were the most obese, and we have seen that the mother plays an essential role in treatment success. This fact is also interesting in that it suggests that the influence of the mother concerning the development of healthy dietary habits extends into puberty.
Another factor that may influence the response and adherence to treatment is the degree of obesity of the children under study. As noted by Feliu et al., children with high BMIs show worse adherence and response to obesity treatment.15 A high percentage of the analysed sample had severe obesity, as our study was conducted in a specialty clinic, and thus the results of this study should only be applied to children of equal anthropometric characteristics. Thus, we still need to find out whether parental BMIs have a similar influence on the response to obesity treatment of children with less severe obesity, most of whom are probably being monitored by primary care paediatricians.
In conclusion, this study corroborated that a high percentage of children that are very obese have obese parents, and that mothers have substantial influence on the adherence and response to obesity treatment in their children, at least if they have a significant degree of obesity. For all the above reasons, this study suggests the need to consider new therapeutic approaches against obesity that involve the entire family unit and the collaborative effort of endocrinologists and paediatric endocrinologists.
Conflicts of interestThe authors have no conflicts of interest to declare.
| Lifestyle and dietary recommendations |
|---|
| 1. Have 5 meals a day with no snacking between meals |
| 2. Do not skip meals, have breakfast every day |
| 3. Have five pieces of fruit or vegetables a day |
| 4. Drink water, no sugary drinks |
| 5. Exercise for 1h a day |
| 6. Limit the number of hours spent watching TV and playing videogames |
| 7. Eat mostly foods in the on-demand and low-calorie groups |
| 8. Avoid very high-calorie foods |
| On-demand foods: cabbage, pepper (spice), chard, peppers, water, Brussels sprouts, leek, artichoke, diet soft drinks, celery, cauliflower, radish, aubergine, spices, watercress, endive, mushrooms, broccoli, escarole, tomato, soy bean sprouts, asparagus, vinegar, courgette, spinach, carrot, pumpkin, green bean, vegetable broth, lettuce, onion, lemon, cucumber |
| Low-calorie foods: shellfish, green pea, boiled pasta, bread (pita, loaf, sliced), biscotti, potato (roasted, boiled, baked), fresh fruits, fresh fruit juices, turkey (skinless), rice (boiled), egg, tuna canned in water, Serrano ham, ham, fresh or frozen fish, squid (no oil), non-fat and low-fat milk, skinless chicken, goat, lentils, sugar-free cereal, pork tenderloin, fresh low-fat cheese, cherries, fresh corn, beets, low-fat cream cheese, rabbit, mango, vegetable purée, fat-free soup, rice salad, lean beef, pasta salad, low-fat yoghourt, rice crackers, Marie biscuits, chickpeas |
| High-calorie foods: avocado, creme brulee, duck, fried chicken wings, frankfurters, fried or breaded fish, whole-fat sugared rice pudding, fruits canned in syrup, pork and beef liver, lamb shank, sunflower seeds, fish sticks, fried egg, cake, whole-fat dairy products, fried squid, fried or breaded chicken or chicken with its skin, cannelloni, cream-based sauces, fatty minced meat, cupcakes, soft or hard cheeses, pork shoulder, custards and flans, cereals with added sugar or cocoa, popcorn, soft drinks, pork belly, spring rolls, chops, coconut, pastries, ribs, pies, juices with added sugar |
| Very high-calorie foods: cured meats (chorizo, salami), honey, sunflower oil, blood sausage, almonds, chocolate biscuits, cocoa spread, hazelnuts, butter biscuits, olives, sugar, ice cream, bacon, sweets, peanuts, lard, French fries, milk chocolate, butter, potato chips, margarine, patés, peanut butter, mayonnaise, aioli sauce, cream cheese, cream, marzipan, tarts, cheese dip, marmalade and jam, ketchup |
Please cite this article as: Regueras Santos L, Díaz Moro A, Iglesias Blázquez C, Rodríguez Fernández C, Quiroga González R, de Paz Fernández JA, et al. Tratamiento de la obesidad en la consulta de endocrinología de un hospital. Influencia del índice de masa corporal de los padres. An Pediatr (Barc). 2015;83:297–303.
Previous presentation: This study was presented at the XXXVI Congreso de la Sociedad EspaÒola de EndocrinologÌa Pedi·trica. (SEEP), 14–16 Mayo 2014 Sevilla.